It’s hard to find a medical institution with no electronic workflow. But not all of the systems that maintain this workflow are smart. With smart EHRs, healthcare entities can utilize extended search options, data from wearables, and smart recommendations.
What is EHR?
The electronic health record software is an integrated repository solution that stores data about all healthcare assistance that a certain patient received during all their life. It documents the who, what, why, when, where, and how of their interactions with medical entities.
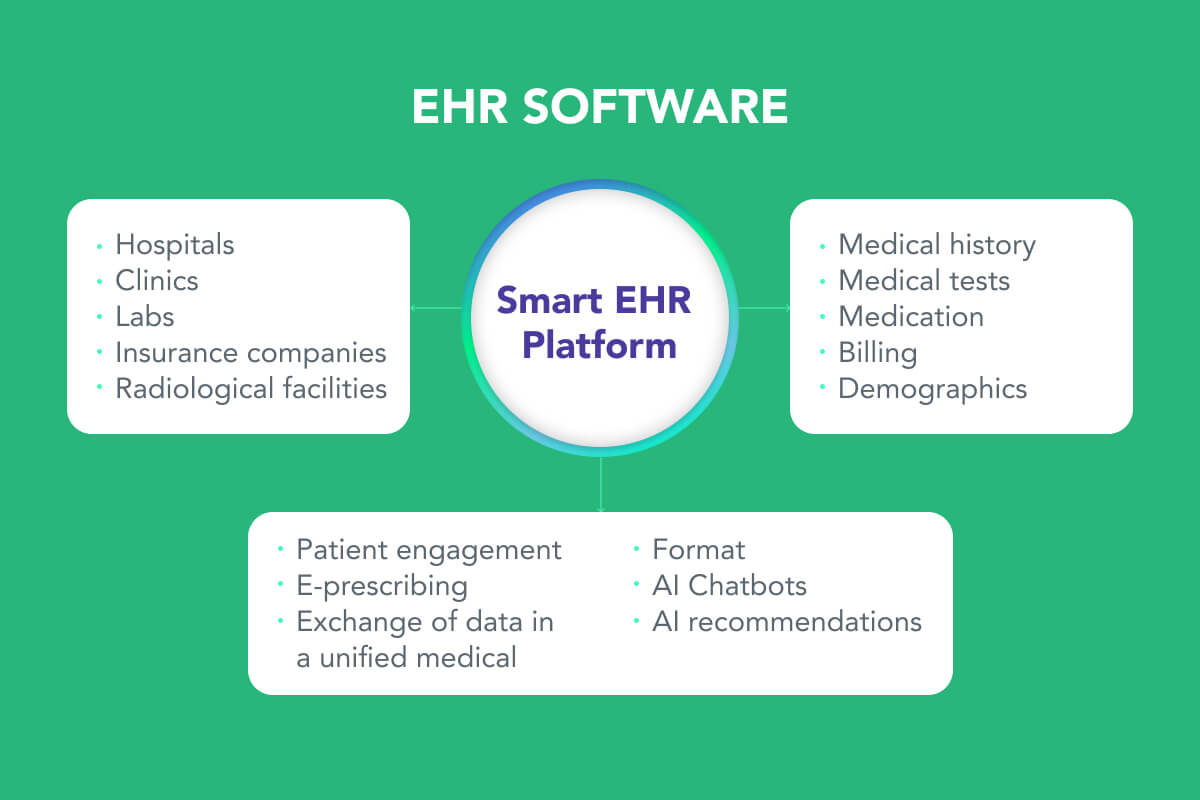
As well, EHR can denote one particular record or name of an individual in this repository. Smart healthcare includes many parties, such as doctors, patients, hospitals, and insurance agencies. It stores and manages a huge volume of data, such as medical history, lab tests, and demographics.
It has many functions, such as searching, reporting, and sharing. And it is used for a number of reasons, for example, disease diagnosis, treatment, hospital management, and health self-management.
What Makes an EHR Smart?
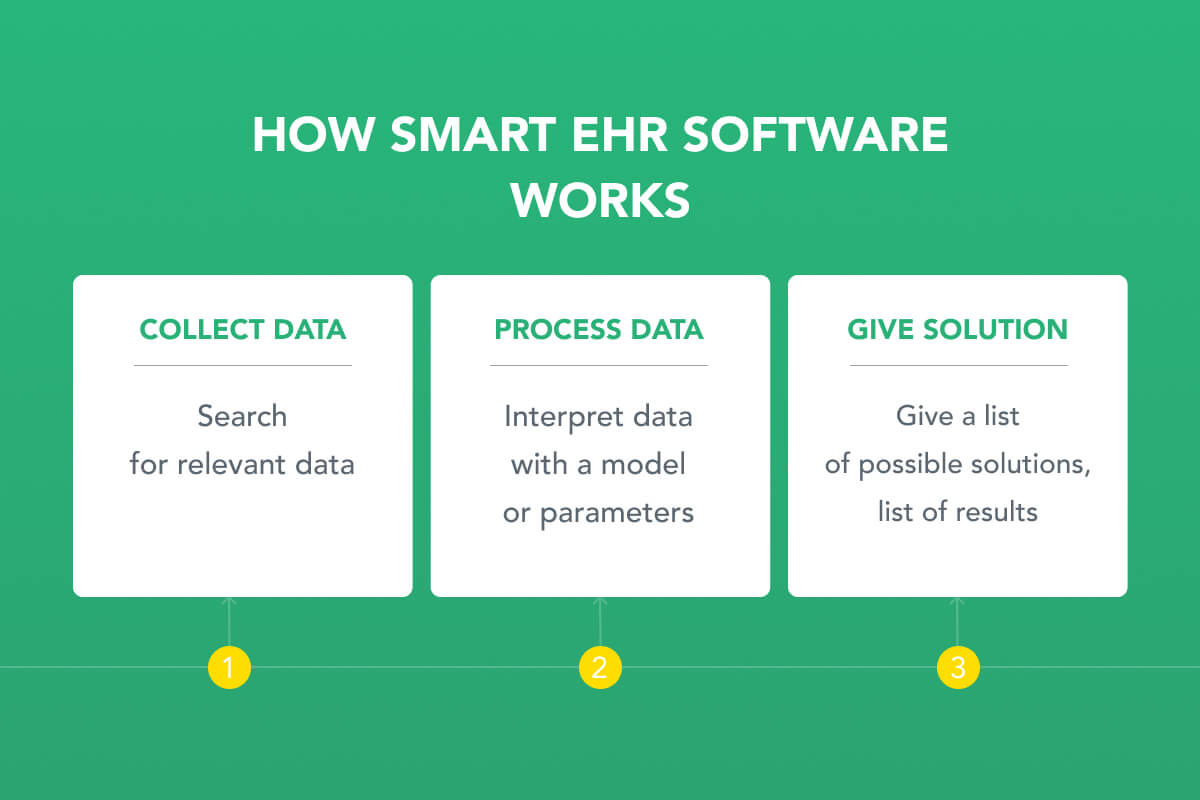
Many scientists research how AI can change the digital organization of healthcare. For example, EHR Intelligence offers its musings on this point. But generally speaking, smart systems can be defined in these terms.
- Smart EHR applies AI algorithms;
- Smart EHR is usually a cloud solution with huge storage and scalability;
- Smart EHR uses a Virtual record of an individual;
- Smart EHR uses context management and extended searches;
- Smart EHR offers possible diagnoses and solutions;
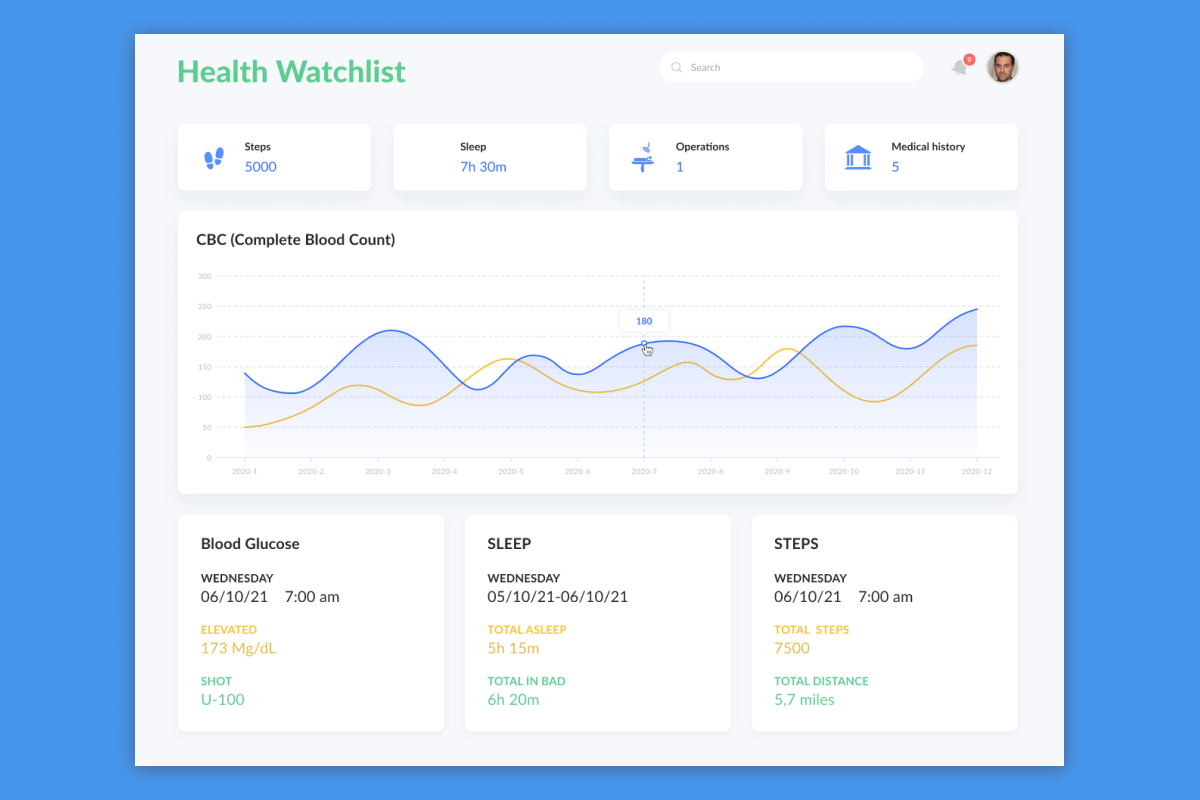
- Smart EHR integrates IoT health solutions such as medical wearables;
- Smart EHR can connect wearables and mobiles.
To design the architecture of smart platforms, developers need to combine providers’ software with AI models. These platforms will be patient-centric.
How Smart EHR Software Works
EHRs are not the sole systems that operate patient data. There is another popular solution that works with this data, stores it, and manages it.
What is the Difference Between EHR and EMR?
EMR software represents the repository that stores medical charts of patients under one practice. Also, EMR can apply to one particular chart of a patient in this system.
This makes EHR software principal storage of patients’ information. EHRs can integrate HMR solutions.
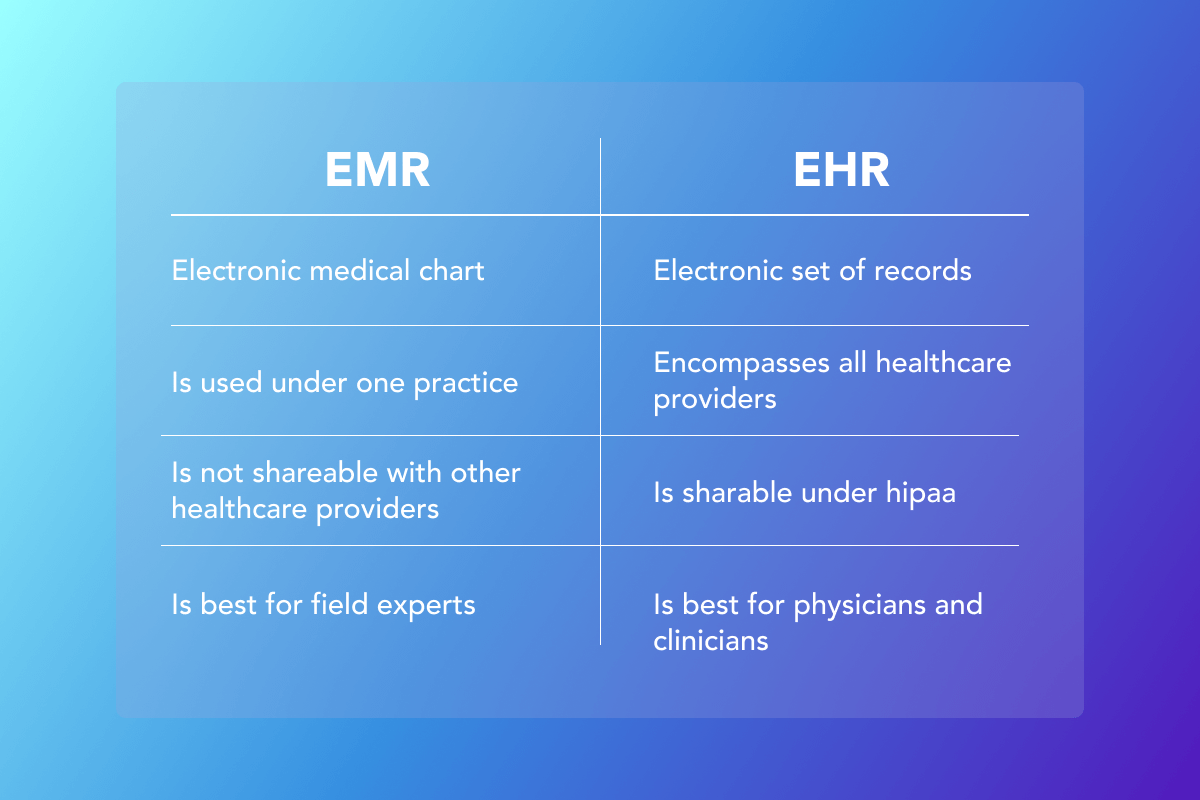
Did you know? Cancer treatment results are stored in EMRs, not EHRs.
What Data is Stored in EHR?
These systems are huge storages of complete, accurate, and current data about patients.
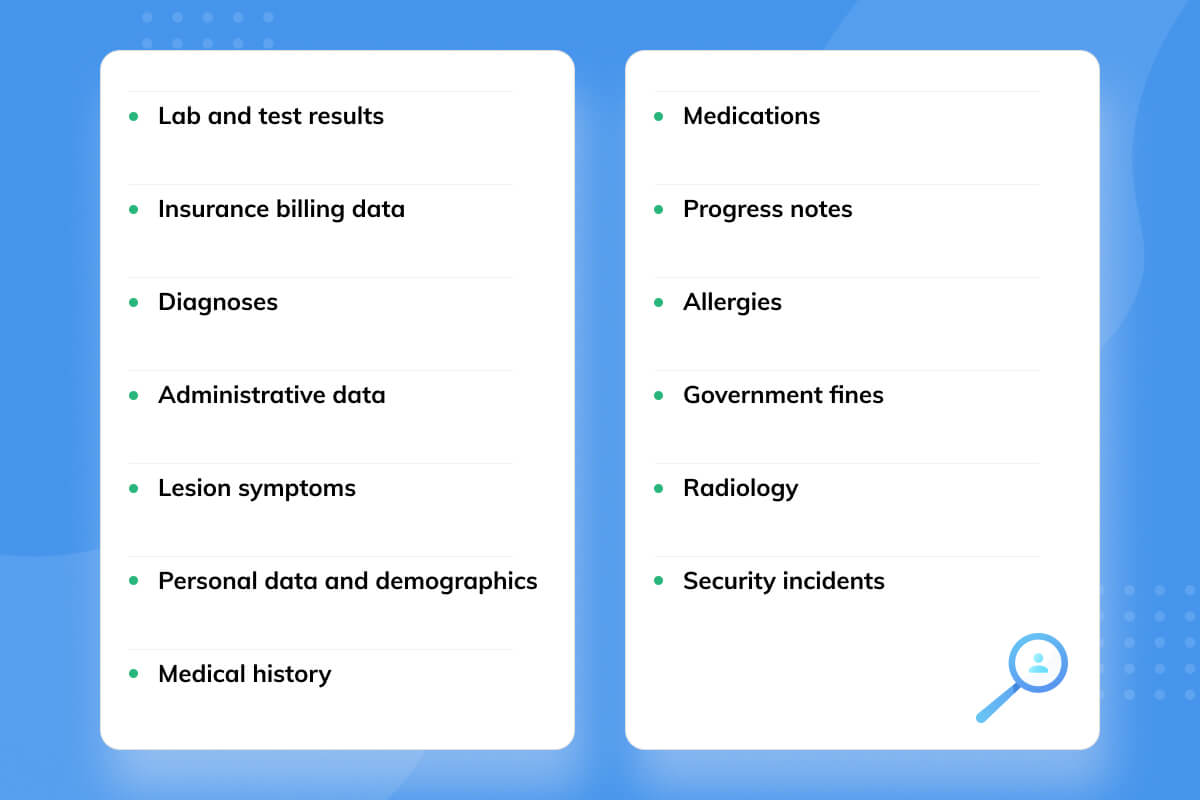
Judging by this list, EHRs treasure the collection that can make Dr. House quit sending investigation groups to unconscious clients. That is why General Practice and Family Practice physicians and clinicians are keen on EHRs. It goes without saying that storing massive volumes of this data requires certain rules.
Compliance with Regulations for the EHR
The state protects PHI (protected health information) with a list of rules such as FHIR, HIPAA, CCR, CCA, DICOM, CCD, SNOMED, and HL7.
Fast Healthcare Interoperability Resources
The FHIR standard:
- Describes the structure where data should be stored;
- Defines how the information must look;
- Describes APIs to send this data.
In their turn, EHRs must enter the required information into this structure.
Smart EHRs protect their data in a number of scenarios, for example:
- Define how to start 3rd-party applications in EHR;
- Identify the EHR user who is using an application;
- Identify particular data that was accessed by this user.
This means that all outer applications and their users will be granted certain permissions to interact with EHR or none. If somebody enters the system via an application, the system will always know who this person is. If this person is searching for data and accessing it, the solution will know exactly what data was in the target. If providers are FHIR compliant, they can feel secure about their information and receive no fines.
Health Insurance Portability and Accountability Act
Under HIPAA regulation, EHR data is considered PHI. This means that all EHR providers should be HIPAA compliant.
3 Rules of HIPAA:
- The Privacy Rule;
- The Security Rule;
- The Breach Notification Rule.
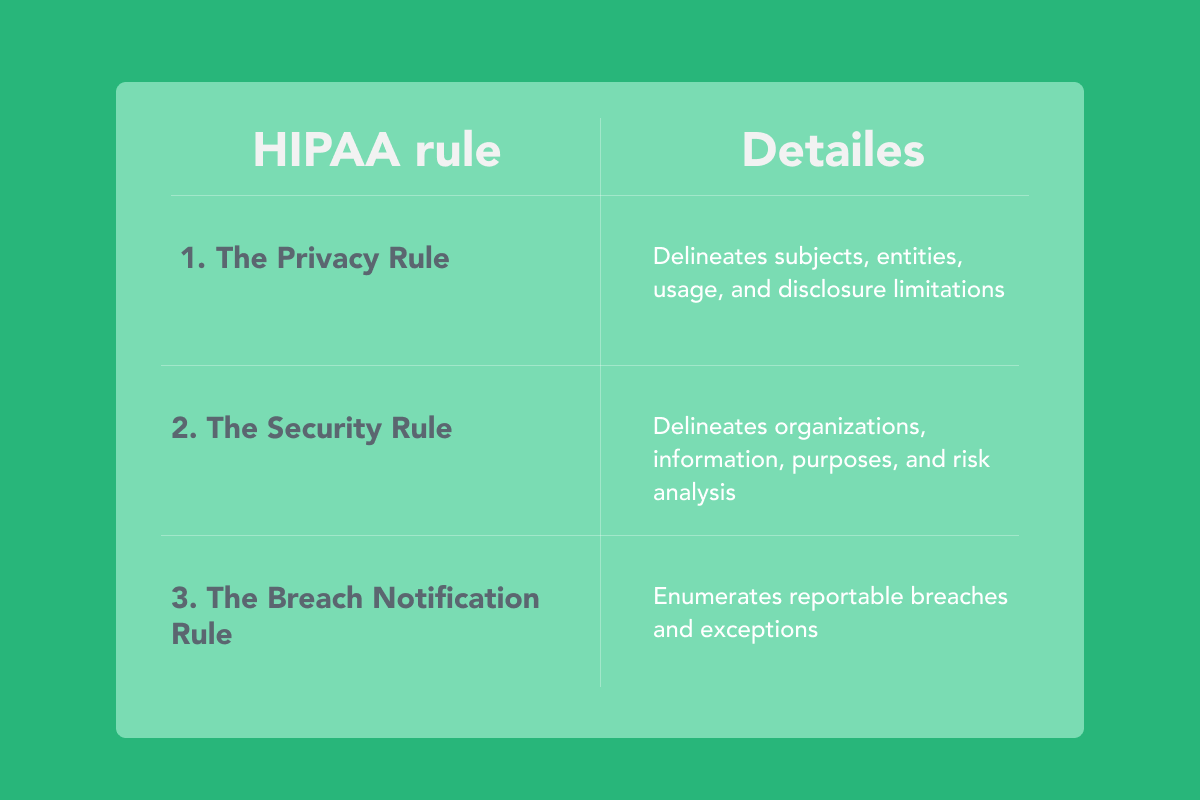
In this way, HIPAA safeguards the patient’s reputation. Even though the systems can comply with the regulations and offer agreeable solutions, they can still have concerns.
Typical Challenges of EHR
Any entity that is going to install an EHR platform or integrate into it should avoid the three “No’s” of EHR.
- Inaccuracies in EHR systems;
- Too complicated systems;
- Not customer-centric EHR developer-companies.

In real life, these points can cause the following situations:
1. Ethical Matters
Overly initiative EHRs can behave insensitively toward doctors. They can send push-up notifications, reminders, and emails to doctors about events. In many cases, they cannot change these settings.
2. Clumberred Graphical Interfaces
If an EHR is not custom-made, its GUIs are unified and can be misleading for particular healthcare entities.
3. Delays in Integrated Systems
Complicated systems with a lot of integrations theoretically should work. But in real life, they encounter inaccuracies. If a doctor sends an order to a lab for tests, the lab’s system can get it with delay. And in some cases, getting a test result a day later can be fatal.
4. Malfunction of Specific Modules
EHRs consist of complex systems such as billing. And they can have issues. Entities can waste $38 million due to uncollected overdue bills and problems with insurance companies. These are the issues that providers have to forecast and avoid in EHRs.
Benefits of EHR/EMR
Bodies that protect human health and parties, who are involved in these services, migrate to EHR or EMR. Mainly because these systems offer electronic workflow, exclude fines, and have lots of integrations.
Grandviewresearch informs that:
CAGR of the global EHR market is expected to go up 3.7% from 2021 to 2028.
Here is the list of benefits that providers can get with health and medical records management systems:
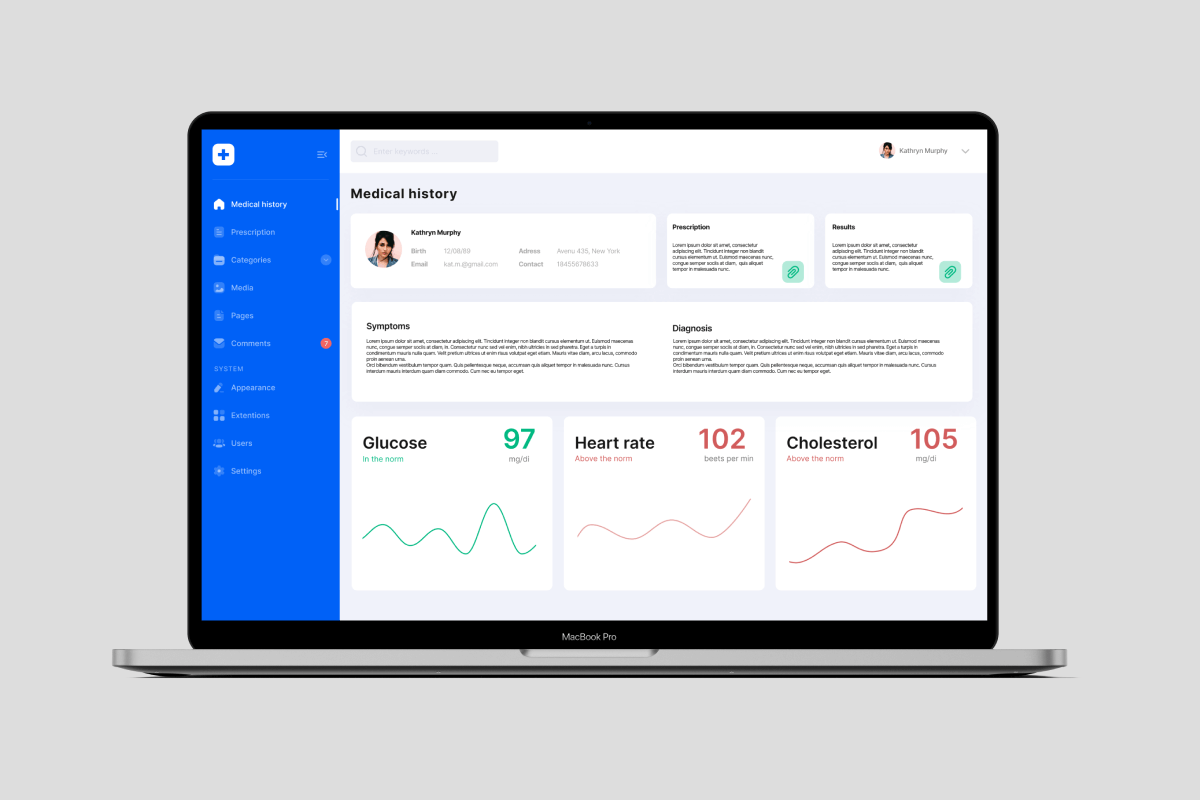
1. Desktop Application
Doctors can work in these systems at their desktops in their offices as at workstations. This is their primary use. Whether they see clients, get lab tests, or do the bills, they can do it full-screen.
2. Mobile Application
Providers can use electronic health records applications and EMR apps from their smartphones. In most cases, mobile apps are applied to send alerts to doctors from wearables of critical clients and for remote consulting.
3. Elastic Search
Providers can find all references to their queries in structured and unstructured data. This means that they can find in the system all mentions of a word or phrase, including titles of files and the body of the texts.
4. Telemedicine Application
Medical record management software of a small private practice and big entity record management system allows doctors to communicate remotely with critical clients via any technical means of communication.
5. Custom Solutions
Small and middle-sized entities can have EHR or EMR made on order. In this way, they exclude the challenges that may emerge with the huge platforms and their packages. With custom solutions, they have the systems totally adjusted to their workflow. And they do not need to adjust their workflow to these unified systems.
6. Extended Platforms
Big EHR platforms can cover the growing needs of general hospitals. If their workflow involves dozens of parties and thousands of records, these systems are choice #1.
7. Protection of Health Information
EHR solutions can safeguard PHI and all the parties that are concerned about it. EHRs can store, transfer, and delete this data in a secure way with cloud technologies.
8. Revenue Cycle Management RCM
EHR and EMR can automate billing and communication with financial institutions that serve this sector. Usually, they integrate entire systems that focus on these relations.
9. Electronic Practice Management
These systems let doctors organize their practice in an electronic way, not as paperwork. Paper workflow in the healthcare sector gradually retires.
10. Book Appointments
These systems also let the patients book their visits to their specialists. They can see available time slots and choose the time that is most convenient for them.
11. Electronic Documentation Management
In these applications, entities can work with all their documents: histories of clients, charts, prescriptions, and statistical descriptions of their results. They can feel secure under the systems that comply with PHI regulations.
12. Time Management and Scheduling

In a health records app and in a medical record management system, doctors can allocate time for events and automatically notify all parties involved about them.
13. Open API and Exchange of Files in a Unified Medical Format
Via open APIs, providers can share unified medical records among systems: medical images and examinations. This can dramatically save providers’ time and streamline medical services to patients.
14. Interoperability Among Healthcare Providers
These systems represent a place for communication among providers in different sectors and facilities: radiology, labs, and hospitals. Doctors can send a request for a medical test or examination to a lab.
15. Reporting and Optimizing Administrative Workflow
Providers can report in an electronic way that reduces the time for minutes and meetings.
16. EHR/EMR Integration
EHR can integrate EMR and many other healthcare systems, making it a single-source holistic solution for patient care.
17. Integration of Wearables
Doctors can receive health information of critical patients from their heart rate and other wearables directly to the EHR desktop or smartphone app.
18. E-Prescribing
When a prescriber is seeing a patient, they can send the medicine prescription to a pharmacy from their e-Prescribing (eRx) service.
19. Questionnaires and AI Chatbots for Patients

Healthcare providers can automate the collection of patients’ health information for preventive reasons. Via these systems, they can email their forms to patients. Or they can apply AI chatbots to interview them.
20. Easier Management of Healthcare Entities
With the electronic workflow, administrative personnel of healthcare facilities has less trouble controlling the general situation in their realm.
Conclusion
Smart EHR solutions represent common EHRs enforced with IoT and AI algorithms. They are local and general principal repositories of patient information. They are also an environment for electronic workflow in the healthcare sector. These systems are mostly meant for general practice physicians and family doctors in large healthcare entities. Smart systems offer many functions in prevention, diagnosing, treatment, research, exchange, reporting, protecting, and billing. These functions can include the free transfer of unified medical data, AI diagnosis, and solutions, integration of wearables, telemedicine, AI questionnaires, extended search, and automation of billing.





